Assam slowly but steadily inching towards zero snake bite deaths
Assam's comprehensive snakebite management model has led to a significant reduction in fatalities, setting a benchmark for the nation. Public awareness and improved healthcare facilities have been key to this success.
- Dec 06, 2024,
- Updated Dec 06, 2024, 3:22 PM IST
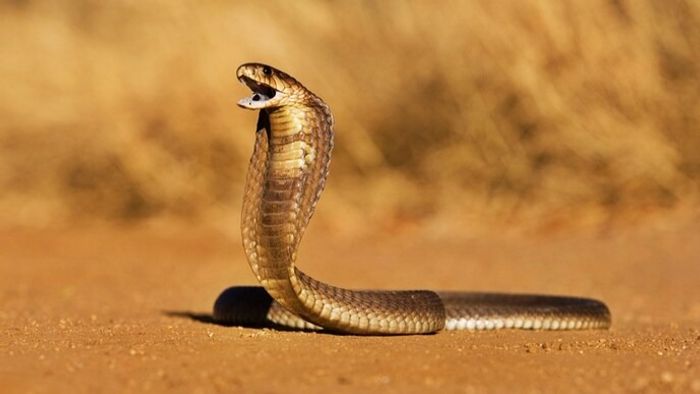
Snake bite is called poor men’s acute health emergency. India is World's 'Snakebite Capital' with 2.8 million bites a year with 35,000–50,000 people dying per year according to World Health Organization (WHO) [1,2]. Lack of a coordinated comprehensive care in snake bite management is the key factor of highest numbers of deaths and morbidity in India and Assam.
India and our state, Assam too lacks comprehensive care model in snake bite management. But we are happy with the progress of our state activity in the year 2024.
Comprehensive care is a planned coordinated preventive, promotive, curative, mental and socioeconomic care to snake bite victims. India lacks the coordinated movement of snake bite victims from field to hospital.
Why India and Assam need a comprehensive care?
1. Lack of awareness amongst public.
2. Majority attended faith healers [3,4].
3. Poorly trained health care workers (HCW) in rural districts [5,6]. Fear of HCW to administer ASV (Anti snake Venom).
4. Poor transportation system to hospital.
5. Delayed ASV administration [7,8]
6. No support to victim’s family due to huge financial burden [9], if treatment is prolonged.
7. No address to mental issues post snake bite [10]
8. It is not approached as acute emergency.
9. Myth that snake bite cases can be treated only in tertiary center.
India and Assam have huge gaps from prehospital, point of source hospital to tertiary care hospital. For effective treatment of snake bite victims, we should have an organised care system starting from public to government. We are happy that in this year we are more or so organised. Public should attend nearby Government Community hospital at the earliest. The community hospital also should welcome and effectively manage such victims, and Government should also support community and district hospitals. As it is a rural community problem, rural community health centres of Assam should start treating these victims. Happily, Assam has addressed all components to prevent snake bite deaths in coming years.
Demow CHC comprehensive model:
400km east of Guwahati,(Capital of Assam),Demow rural CHC(Community Health Centre) started a model focusing all component in snake bite management in the year 2018 and successfully treated 2688 numbers of victims with only one death in the year 2020.This rural CHC has achieved zero deaths in the year 2021(464 patients),2022(573 patients),2023(630 patients) and 2024(793 patients till 30th November ).It has following component VRT, FRT& snake bite treatment room.
A. Prehospital management: Venom Response Team (VRT)
Prehospital management is greatly neglected in India due to lack of education of our society. After snake bite our public completely lost and often mislead by the superstitions running in our society. Demow CHC started to educate public since 2008(Fig A). A VRT was constructed to guide snake bite victims in each gram panchayat level comprising gram Sevak, local organizations & ASHA workers. They can activate, communicate HCW & can transfer victims safely to nearest hospital. It is the need of the hour. Demow model is focused to educate, empower, and train public. These trained/educated public are called VRT.
Public awareness & Education is the key.
We must take help of 3Ps.Public, Press & Politician. Now a days, digital platform is the best to reach out many within short span of time. We must publish our own successful stories in our own local language in various digital formats. Facebook and what’s app are the most popular digital media in various nook and corners of India, we should post our success stories of venomous snake bite treatments. Let public know that snake bite means hospital admission. Make them believe that there is a full proof medical management of venomous/nonvenomous snake bite in India. We have completed 500 numbers of community awareness on 30th November 2024 in Borhat,Charaideu district. Assam Government is now focusing on public awareness in the form of pamhlets,newspaper or radio advertise encouraging public to attend nearby CHC.ASHA health care workers who are very close to rural community are trained and encouraged to transfer nearby CHC at the earliest.
B. Strengthening the health care system :FRT & snake bite treatment room
Strengthening of our rural primary (PHC) and community health Centre (CHC) is the key in our model. It is true that bites from Cobra, we may not get time. From 0hrs-3hrs, patient may develop fast neurotoxic symptoms. People staying in remotest village and transfer such victims from CHC to district hospitals without ASV administration may kill these groups of patients during transportation. Point of source identification (at PHC and CHC level) of venomous snake bite symptoms and administration of ASV (and neostigmine in neurotoxic) will definitely prevents many deaths in India, which as rural CHC (Demow)have proved it since year 2018. Even if patients come late to hospital with full blown symptoms to a PHC, our HCW should be educated and trained enough for simple maneuver like bag and mask ventilation and transfer with ASV. Demow CHC, health care workers can identify the early danger symptoms and signs and can administer ASV or neostigmine or basic airway management in snake bite room. A dedicated snake bite room was opened on the year 2020,where the hospital has kept all necessary medications including ASV and basic equipments in an organized way so that everybody on duty can treat snake bite victims confidently. Snake bite room also contain photo of the venomous snakes for identification by the victim, which helps the on-duty health care workers in treatment. These trained health care workers are called fast response team (FRT).
Demow CHC comprehensive model : can be a model for India
Demow CHC successfully formed a non-breakable chain from community to hospital. Any snake bite incident, victim or his/her family reports to local VRT(Venom Response Team).VRT Team will provide prehospital management. They will communicate and activate Demow hospital. Means before the patient reaches hospital, hospital staff are aware about the incident. Sometimes VRT uploads the snake photo or bitten limb in what’s app. They discourage tourniquet and transfer the victim with immobilization of the limb. Within 20 minutes to 1 hr. victims usually reaches hospital and kept in hospital for 24hrs.
Hospital staff assesses the situation, treats in CHC itself on early sign and symptoms with ASV, neostigmine & glycopyrrolate. If needed patients is transferred to nearby tie up ICU with bag & mask ventilation. Simultaneously, FRT Communicates & activates the tertiary care Centre. Till now this CHC has shifted only two victims of krait bite for mechanical ventilation(artificial respiration). Both are doing fine. Out of these two, one was 3month pregnant lady. As of now both mother and womb baby are doing fine, and we are planning for caesarian section in February 2025.Cobra and krait venom causes descending paralysis. This venom First attacks the cranial nerves(central nervous system nerves) and slowly progresses to neck and respiratory muscles of chest and diaphragm(major muscle of respiration). As in this hospital, victims attend immediately and admitted for observation, once the neurotoxin attacks cranial nerves it causes certain symptoms like difficulty in swallowing, dysarthria(difficulty in talking),blurring of vision, among others. This is called the golden time for health care workers. At this symptom, the FRT immediately infuses ASV and prevents further descends of venom and ultimately prevents paralysis of respiratory muscles. If respiratory muscles are not paralysed, definitely patient does not require any ICU or artificial respiration.
The Demow Model VRT, FRT, Snake bite treatment room has been presented in International Toxinology conference, Singapore 2024,Venom and Toxin conference, Oxford 2022 and NAPSE 2024 (National Action Plan for snake envenoming) launch programme in New Delhi. NAPSE 2024 has endorsed Demow CHC idea of snake bite treatment room.
Our suggestions for zero death in Assam involving government and policy makers as without them it is near impossible to solve the problem.
1. One class/session should be included in MBBS curriculum especially in 5th year (last year) of MBBS training. This class should be taken by a physician who is regularly treating a snake bite victim and by a herpetologist, as there are differences of venomous snakes in different part of India. Notably Saw scaled viper and Russel Vipers are not available in Assam. But however, in some areas of Bongaigaon, Chirang and Tezpur districts few numbers of Russel Vipers were reported recently. First reported Russel viper bite was in the year 2016 followed by in the year 2023&2024. Total Eight numbers of Russel viper bite are reported Seven were from Bongaigaon district (lower Assam adjacent to Bhutan and West Bengal border), and one number was from Tezpur district. Out eight reported Russel viper bite, two died. After passing out of MBBS and internship, they should do compulsory rural posting in different rural health centers, as per Government bond. If we can train/teach them at MBBS level, the fear to handle snake bite victims will be less at point of source (PHC/CHC level). If we start treating victims at PHC/CHC level, many mortalities and morbidity will be prevented. We have observed that emergency departments are most of the time are run by just passed out Interns and as they are not trained in this subject, many a time they miss early clinical symptoms, causing unfortunate deaths. Therefore, a class/session at last year of MBBS will greatly help them to train in the subject.
2. All government hospital should have a dedicated snake bite room adjacent to emergency department.
3. Yearly update of HCW about snake bite management.
4.Referral to higher center should be stopped unless indicated.
5.Snake bite victims should be approached as acute medical emergency, like road traffic accident.
Ten reasons why Assam can achieve zero deaths by 2026:
1. Assam has identified venomous snakes of this region.
2. Assam has studied the venom of these venomous snakes.
3. In Tezpur University and IASST(Institute of Advanced Study in Science & Technology),Guwahati venom study is going on.
4. Assam has its own Assam specific SOP.
5. Assam has trained 1500+ MO of all districts & started treating victims at source level
6. Upto CHC level ASV and other logistics are available.
7. Few remote PHC also has ASV and logistics.
8. Public started to visit nearby rural hospitals instead of faith healers.
9. Government of Assam is supporting its doctors.
10. Mapping of all districts of Assam in relation to prevalent venomous snakes done(according to patient turnover to hospitals)
In collaboration with the government of Assam, 1500+ numbers of medical officers from community health centre and district hospitals were trained in phased manner under NHM(National Health Mission),Assam. Thanks to the effort of MD, NHM, Assam & State Nodal officer Dr S.A. Laskar. Collaborative efforts from Government of Assam & medical officers have prevented 70 per cent deaths in the year 2023 in comparison to year 2022.This year, Assam have reported 35 numbers of death, and our health care workers has saved 1550+ numbers of venomous snake bite victims in different CHC,PHC and district hospitals.
In collaboration with NHM, Assam, we have prepared a roadmap to achieve zero death by the year 2025-2026.Hoping a best result very soon. Assam has launched its Assam specific SOP on 23rd of November 2024.Previously Tamil Nadu and West Bengal has launched its own SOP. But Assam is the first state to slightly modify the existing National guidelines in snake bite management based on various venom studies of Assam venomous snakes and clinical data of 5000 plus snake bite patients from different CHC/PHC/District hospitals of Assam.
In 2022, in Assam there was 100+ deaths & snake bite reporting was also some hundred only vs 10,000 numbers in 2024. Due to collaborative efforts from Doctors & health care workers of Assam, Snake rescuers of Assam and Assam Government, the death numbers were reduced to 37 in 2023 and 35 in 2024. We have analysed all deaths and we have identified the lacunae and we are collectively worked on these lacunae and we are determined to solve these lacunae in year 2025.We are heading towards zero death as an unit.
Definitely Assam is inching towards zero deaths. Overall, Assam is a leading example in India for its successful implementation of a comprehensive snakebite management program.
References:
1. Chippaux JP (1998) Snake-bites: appraisal of the global situation. Bull World Health Organ 76: 515–524.
2. Kasturiratne A, Wickremasinghe AR, de Silva N, Gunawardena NK, Pathmeswaran A, et al. (2008) The global burden of snakebite: a literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS Med 5: e218.
3. Simpson ID (2008) A study of the current knowledge base in treating snake bite amongst doctors in the high-risk countries of India and Pakistan: does snake bite treatment training reflect local requirements? Trans R Soc Trop Med Hyg 102:1108–1114.
4. Chauhan S (2005) Pre-hospital treatment of snake envenomation in patients presented at a tertiary care hospital in northwestern India. J Venom Anim Toxins incl Trop Dis 11:275–282.
5. Bawaskar HS, Bawaskar PH (2002) Profile of snakebite envenoming in western Maharashtra, India. Trans R Soc Trop Med Hyg 96:79–84.
6. Hati AK, Mandal M, De MK, Mukherjee H, Hati RN (1992) Epidemiology of snake bite in the district of Burdwan, West Bengal. J Indian Med Assoc 90: 145–147.
7. Suchithra N, Pappachan JM, Sujathan P (2008) Snakebite envenoming in Kerela,south India:Clinical profile and factors involved in adverse outcomes.Emerg Med J 25:200-204.
8. Narvencar K (2006) Correlation between timing of ASV administration and complications in snake bites. J Assoc Physicians India 54: 717–719.
9. Sakthivel Vaiyapuri et al.Snakebite and Its Socio-Economic Impact on the Rural Population of Tamil Nadu, India.PLoS One.2013:8(11):e80090.
10. Bhaumik S, et al. BMJ Global Health 2020;5:e004131. doi:10.1136/bmjgh-2020-004131