COVID-19 most severe among all declared global emergency, says WHO
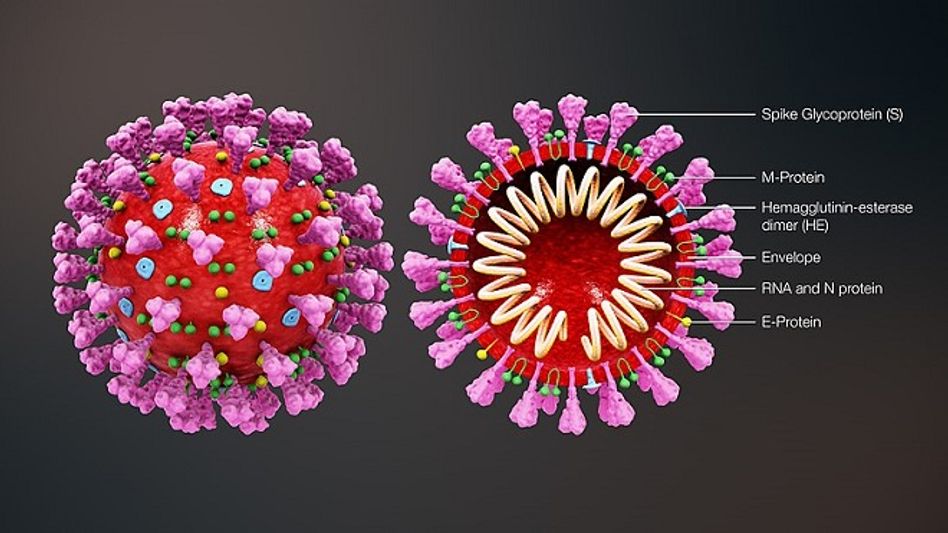 Source: Wikimedia Commons
Source: Wikimedia CommonsWHO director Tedros Adhanom spoke on the issue of COVID-19 who highlighted that "COVID-19 is easily the most severe".
This Thursday marks six months since WHO declared COVID-19 a public health emergency of international concern.
This is the sixth time a global health emergency has been declared under the International Health Regulations, but it is easily the most severe.
Almost 16 million cases have now been reported to WHO, and more than 640,000 deaths.
And the pandemic continues to accelerate.
In the past 6 weeks, the total number of cases has roughly doubled.
When I declared a public health emergency of international concern on the 30th of January – the highest level of alarm under international law – there were less than 100 cases outside of China, and no deaths.
Also read: Does China eye Himachal after Ladakh stand-off?
As required under the International Health Regulations, I will reconvene the Emergency Committee later this week to re-evaluate the pandemic and advise me accordingly.
COVID-19 has changed our world. It has brought people, communities and nations together, and driven them apart.
It has shown what humans are capable of – both positively and negatively.
We have learned an enormous amount, and we’re still learning.
But although our world has changed, the fundamental pillars of the response have not: political leadership, and informing, engaging and listening to communities.
And nor have the basic measures needed to suppress transmission and save lives: find, isolate, test and care for cases; and trace and quarantine their contacts.
Keep your distance from others, clean your hands, avoid crowded and enclosed areas, and wear a mask where recommended.
Where these measures are followed, cases go down. Where they’re not, cases go up.
Countries and communities that have followed this advice carefully and consistently have done well, either in preventing large-scale outbreaks – like Cambodia, New Zealand, Rwanda, Thailand, Viet Nam, and islands in the Pacific and Caribbean – or in bringing large outbreaks under control – like Canada, China, Germany and the Republic of Korea.
These are just a few examples, but there are many more that could have been listed.
The bottom line is that one of the most fundamental ingredients for stopping this virus is determination, and the willingness to make hard choices to keep ourselves and each other safe.
Over the past 6 months, WHO has worked tirelessly to support countries to prepare for and respond to this virus.
I am immensely proud of our organization, WHO, and its incredible people and their efforts.
Within days of learning of the first cases in China, we published extensive guidance on how to find, test and treat cases and protect health workers.
We also published the first protocol for testing for the virus, and immediately started working with a manufacturer in Germany to produce tests and ship them to countries most in need.
We convened hundreds of scientists to develop a roadmap for research.
We have brought together thousands of experts from all over the world, in many disciplines, to analyse the evolving evidence and distil it into guidance.
Never before has WHO produced such a large volume of technical advice in such a short period.
More than 4 million people have enrolled in our training courses through the OpenWHO.org online learning platform.
We launched the Solidarity Trial to find answers fast about which therapeutics are the most effective.
We launched Solidarity Flights to ship millions of test kits and tons of protective gear all over the world.
We launched the Solidarity Response Fund, which has so far mobilized more than US$225 million from more than 563,000 individuals, companies and philanthropies.
In addition, we mobilized more than 1 billion dollars from Member States and other generous donors to support countries.
We worked with community organizations, religious groups, the public and private sectors, tech companies and many other groups to fight the infodemic.
And we have formed the ACT Accelerator to speed up the development, production and equitable distribution of vaccines, diagnostics and therapeutics.
We have done an incredible amount, but we still have a long, hard road ahead of us.
And we know that the impacts of the pandemic are felt far beyond the suffering caused by the virus itself.
Many essential health services have been disrupted, including for hepatitis.
Tomorrow is World Hepatitis Day.
There are five main strains of the hepatitis virus.
The two most common types, B and C, cause liver damage and liver cancer.
An estimated 325 million people globally live with hepatitis B or C, and each year these viruses kill an estimated 1.3 million people.
In 2016, the World Health Assembly adopted the global hepatitis strategy, setting the world’s first hepatitis elimination targets.
The strategy calls for the elimination of viral hepatitis as a public health threat by 2030 – reducing new infections by 90% and mortality by 65%.
Even talking about hepatitis elimination would have once seemed a fantasy.
But new drugs have transformed hepatitis C from a lifelong, deadly disease into one that in most cases can be cured in 12 weeks – although in many countries the medicines remain expensive and out of reach for many patients.
Still, many countries are making incredible progress.
Egypt has tested more than 60 million people for hepatitis C, and linked those who test positive to treatment free of charge.
We are also seeing some progress with hepatitis B elimination, for example in Asia where childhood hepatitis B immunization coverage is high, including the all-important birth dose.
Today we are celebrating more good news:
New research led by WHO and the London School of Hygiene and Tropical Medicine shows that together we have achieved the global target set in 2000 to reduce the prevalence of hepatitis B infections in children under five years of age to less than 1% by 2020.
This landmark achievement means we will dramatically reduce the number of cases of liver cancer and cirrhosis in future generations.
However, progress is being hampered by low coverage of hepatitis B vaccine in some regions, particularly in sub-Saharan Africa, where many children still miss out on the all-important vaccine dose at birth.
One of the most significant challenges we face in eliminating hepatitis B is mother-to-child transmission.
Tomorrow, WHO is launching new guidelines for the prevention of mother-to-child transmission of hepatitis B.
We call on countries – especially those with the highest burden – to implement these new guidelines as an important stepping stone on the road to hepatitis elimination.
That road has been made harder by COVID-19.
Services for prevention, testing and treatment have been disrupted, supply chains are being interrupted, limited financial and human resources are being diverted and the political focus has shifted to containing the pandemic and economic recovery.
All of which means there is a real risk we could lose the gains we have made.
Like so many diseases, hepatitis is not just a health problem. It’s an enormous social and economic burden.
As we mark 6 months since the declaration of the global health emergency, the COVID-19 pandemic is illustrating that health is not a reward for development, it’s the foundation of social, economic and political stability.
We are not prisoners of the pandemic. Every single one of us can make a difference. The future is in our hands.
WHO remains totally committed to serving all people and all countries with science, solutions and solidarity.
Readers like you make Inside Northeast’s work possible.
To support our brand of fearless and investigative journalism, support us HERE.
Download:
The Inside Northeast app HERE for News, Views, and Reviews from Northeast India.
Do keep following us for news on-the-go. We deliver the Northeast.
Copyright©2025 Living Media India Limited. For reprint rights: Syndications Today









